The Effect and Mechanism of the Effect of Alcohol on Bacteria
In our daily lives, alcohol is frequently encountered as a common antiseptic agent. It is ubiquitous in medical settings, household cleaning products, and personal hygiene solutions. Despite its widespread use, many people may not fully understand how alcohol exerts its bactericidal effects or the specific mechanisms of its action against bacterial cells. In this comprehensive article, we will delve into the intricacies of alcohol’s impact on bacteria, exploring how it affects bacterial growth, the underlying mechanisms of its bactericidal properties, and the role that different alcohol concentrations play in influencing bacterial survival.
Understanding How Alcohol Influences Bacterial Growth
The interaction between alcohol and bacterial cells can vary depending on several factors, including the type and concentration of alcohol. Ethanol and isopropanol are the most commonly used alcohols for antibacterial purposes. Ethanol, particularly, is widely recognized for its effectiveness in inhibiting bacterial growth. When applied to bacterial cultures, ethanol disrupts the cell membranes, leading to cellular leakage and, often, cell death.
Several studies have shown that alcohol can effectively kill a variety of bacteria, including common pathogens such as Escherichia coli and Staphylococcus aureus. By denaturing proteins and dissolving lipids, alcohol compromises the structural integrity of bacterial cell envelopes. This disruption is crucial as it impairs the bacteria’s ability to maintain homeostasis and perform essential life functions.
Interestingly, alcohol’s effect on bacterial growth is not instantaneous; it requires a certain exposure time. For alcohol to be effective, bacterial cells must be in contact with the solution for a sufficient duration, usually a few seconds to a few minutes. The exact timing can depend on factors such as alcohol concentration, type of bacteria, and environmental conditions.
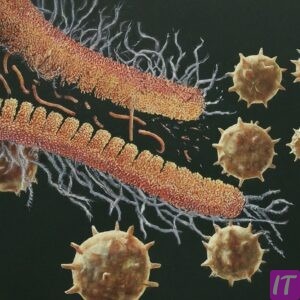
Bacteria in biofilms—communities of microorganisms adhered to surfaces—show different responses to alcohol compared to their planktonic (free-floating) counterparts. Biofilms are known for their resilience and resistance to disinfectants. Consequently, higher concentrations of alcohol or prolonged exposure times might be necessary to disrupt biofilms effectively.
The pH level of the environment also plays a role in alcohol’s bactericidal efficiency. Acidic conditions can enhance alcohol’s ability to denature bacterial proteins, providing an additional mechanism to inhibit bacterial growth. On the other hand, neutral or alkaline conditions might reduce alcohol’s effectiveness.
Temperature is another critical factor that affects how alcohol influences bacterial growth. Warmer temperatures can accelerate the denaturing process of bacterial proteins, thus enhancing the bactericidal effect of alcohol. Conversely, lower temperatures can slow down the interaction and reduce the overall effectiveness of alcohol as an antimicrobial agent.
The presence of organic matter, such as proteins or sugars, in the environment can impede alcohol’s ability to kill bacteria. Organic matter can act as a protective barrier, shielding bacteria and absorbing some of the alcohol, thereby reducing its bactericidal potency.
During the initial contact with bacteria, alcohol causes the outer layers of the cell envelope to coagulate, a process that leads to the formation of a rigid structure. This coagulated layer can sometimes prevent deeper penetration of alcohol, thus necessitating sufficient exposure to ensure bacterial death.
The frequency of alcohol application can also influence bacterial growth. Regular use of alcohol-based disinfectants can help maintain a low bacterial load, but overuse might lead to the development of resistant bacterial strains, which is a concern in clinical settings.
Alcohol’s impact on bacterial metabolism is substantial. It inhibits enzymes involved in essential metabolic pathways, resulting in decreased energy production and an inability for the bacteria to grow or reproduce. The metabolic disruption caused by alcohol significantly contributes to its bactericidal effect.
Bacteria can develop adaptation mechanisms to survive in alcohol-rich environments, such as altering their membrane composition or upregulating stress response proteins. Understanding these adaptive responses is critical for developing more effective antibacterial strategies.
Alcohol’s interaction with bacterial DNA is another area of interest. While it does not directly cause DNA damage, the overall cellular stress induced by alcohol exposure can lead to mutations and impaired DNA replication mechanisms. As a result, this can impair bacterial proliferation.
Some bacteria possess alcohol dehydrogenase enzymes that can metabolize ethanol, potentially reducing its effectiveness. This enzymatic activity, however, is usually not sufficient to confer significant resistance in most bacterial species.
It is apparent that the duration and concentration of alcohol application are key determinants of its success as an antibacterial agent. Ensuring optimal conditions can maximize its bactericidal effects and help maintain an environment that is hostile to bacterial survival.
Unveiling the Mechanisms Behind Alcohol’s Bactericidal Properties
The bactericidal properties of alcohol stem from its ability to disrupt vital cellular processes in bacteria. The primary mechanism involves the denaturation of proteins, which are essential components of all living cells. By unfolding and inactivating these proteins, alcohol prevents bacteria from carrying out necessary functions such as metabolism, replication, and repair.
One of the first targets of alcohol in bacterial cells is the cell membrane. Comprising a lipid bilayer with embedded proteins, the cell membrane serves as a permeability barrier and structural support. Alcohol disrupts the lipid bilayer, leading to increased membrane permeability and leakage of cellular contents.
Protein denaturation caused by alcohol is both swift and extensive. The alcohol molecules interact with protein molecules, destabilizing their three-dimensional structure. This interaction causes proteins to unfold and lose their functional properties, which are crucial for bacterial survival.
Beyond denaturing proteins, alcohol also affects membrane-bound enzymes and transport proteins. These proteins play a critical role in maintaining ion gradients, nutrient uptake, and waste excretion. Inactivating these proteins disrupts essential cellular processes, leading to bacterial death.
Alcohol-induced membrane disruption can also result in the collapse of the bacterial cell wall. This collapse compromises the bacterium’s ability to maintain its shape and protect itself from osmotic pressure, often resulting in cell lysis, where the cell bursts open.
It is important to note that alcohol preferentially targets the outer membrane of Gram-negative bacteria due to their lipid-rich outer layers. Gram-positive bacteria, with their thick peptidoglycan layers, are affected differently. However, both types of bacteria are susceptible to alcohol’s bactericidal effects through protein denaturation and membrane damage.
Alcohol can also interfere with the function of bacterial ribosomes, which are responsible for protein synthesis. By disrupting ribosome structure or function, alcohol inhibits the production of new proteins, restricting the bacteria’s ability to grow and divide.
In addition to membrane and protein damage, alcohol’s interaction with water molecules in the cytoplasm adds another layer of complexity to its bactericidal mechanism. The solvation effect of alcohol leads to dehydration of the bacterial cell, further inhibiting metabolic activities and leading to cell death.
Using high-resolution imaging techniques, researchers have observed the morphological changes in bacterial cells upon exposure to alcohol. These changes include membrane blebbing, cytoplasmic shrinkage, and the formation of amorphous aggregates—all indicative of severe cellular distress.
Alcohol’s ability to induce oxidative stress in bacterial cells is another mechanism worth highlighting. By generating reactive oxygen species (ROS) or interfering with antioxidant systems, alcohol exacerbates cellular damage, hastening bacterial death.
The precise impact of alcohol on bacterial DNA has yet to be fully understood. Nonetheless, it is known that alcohol can indirectly cause DNA strand breaks and impair the repair mechanisms that bacteria rely on to counteract damage from environmental stressors.
For persistent bacterial structures such as spores, alcohol’s efficacy can be somewhat limited. Spores possess highly resilient protective layers, making them more resistant to alcohol. To address this, alcohol can be combined with other disinfectants to enhance its overall bactericidal effect against spore-forming bacteria.
The combined use of alcohol and other antimicrobial agents often results in a synergistic effect. For instance, the addition of quaternary ammonium compounds can enhance alcohol’s penetration and effectiveness, providing a more potent antibacterial solution.
Moreover, alcohol’s volatile nature allows it to evaporate quickly, making it both a practical and effective disinfectant for surfaces and hands. Its quick evaporation also ensures minimal residue, reducing the potential for adverse reactions.
Despite alcohol’s effectiveness, there are limits to its bactericidal capabilities. Specifically, bacteria embedded in organic material or biofilms require higher concentrations and longer exposure times to achieve significant killing effects.
Another challenge lies in the variable sensitivity of different bacterial species to alcohol. While most pathogens are susceptible to alcohol, some environmental or opportunistic pathogens might exhibit resistance, necessitating alternative disinfection strategies.
Understanding the comprehensive mechanisms by which alcohol exerts its bactericidal properties is vital for optimizing its use in various applications. This knowledge can guide best practices in healthcare, food safety, and other fields requiring stringent microbial control.
By continuing to explore the molecular details of alcohol’s interaction with bacterial cells, scientists can develop more effective formulations and protocols to combat a wide range of bacterial infections and contaminations.
The Impact of Alcohol Concentration on Bacterial Survival
The concentration of alcohol is a critical determinant of its effectiveness as an antimicrobial agent. Solutions containing 60-90% alcohol are generally considered the most effective for killing bacteria and other pathogens. This optimal range arises from the need to balance alcohol’s inherent bactericidal properties with its ability to penetrate bacterial cells.
At alcohol concentrations below 50%, the bactericidal effect diminishes significantly. Lower concentrations do not sufficiently disrupt bacterial membranes or denature proteins, leading to higher survival rates among bacteria. These lower concentrations are often ineffective against resistant bacterial strains or biofilm-embedded bacteria.
On the other hand, alcohol concentrations above 90% can be less effective than those within the optimal range. High concentrations can cause rapid protein coagulation on the surface of bacterial cells, forming a barrier that prevents deeper penetration of alcohol into the cell.
Vegetative bacterial cells, those that are actively growing and reproducing, are generally more susceptible to alcohol at concentrations within the 60-90% range. These cells rely heavily on their metabolic functions, which are easily disrupted by alcohol, leading to swift cell death.
Spores, the dormant form of some bacteria, pose a greater challenge. Due to their robust protective layers, even high concentrations of alcohol may not fully penetrate or inactivate spores. In such cases, additional chemical agents or physical methods may be required to ensure complete sterilization.
For hand sanitizers, the recommended alcohol concentration is around 70%. This concentration is effective for killing most pathogens while remaining safe for frequent use on the skin. Higher concentrations might cause skin irritation or dryness without providing significantly improved antimicrobial action.
The interaction between alcohol concentration and bacterial survival can vary depending on the specific type of bacterium. For example, some Gram-negative bacteria may require higher concentrations of alcohol for effective killing compared to Gram-positive bacteria.
Alcohol concentrations must be carefully chosen depending on the intended application. In healthcare settings, higher concentrations may be utilized for surface disinfection, while intermediate concentrations are preferred for hand hygiene practices.
The presence of additional ingredients in alcohol-based solutions can also influence their effectiveness. For instance, adding water to ethanol not only helps prevent rapid evaporation but also enhances protein denaturation and membrane solubilization, thus improving the overall bactericidal effect.
When considering environmental factors, humidity and temperature can impact the efficacy of alcohol at different concentrations. Higher environmental humidity can decrease evaporation rates, allowing alcohol to act for a longer duration. Conversely, lower temperatures can reduce the bactericidal efficiency of alcohol solutions.
In industrial and laboratory settings, the choice of alcohol concentration is often guided by regulatory standards and best practices designed to ensure maximum microbial control. Adhering to these standards is crucial to maintain safe and hygienic conditions.
The efficacy of alcohol against bacterial biofilms, which are notoriously difficult to eradicate, also depends on concentration. Higher concentrations, combined with extended exposure times or mechanical disruption, are generally required to effectively kill biofilm-associated bacteria.
Given these considerations, the formulation of alcohol-based disinfectants must carefully balance concentration with other factors such as volatility, pH, and the nature of the bacterial challenge. Research continues to explore ways to optimize alcohol formulations for enhanced bacterial control.
Further studies are needed to explore the mechanisms by which different alcohol concentrations affect specific bacterial strains, especially those involved in hospital-acquired infections and other resistant forms of bacteria.
The effectiveness of alcohol against certain emerging pathogens, particularly those that form resistant biofilms or have unique lipid compositions in their membranes, remains an active area of research. Tailoring alcohol concentrations and formulations to target these pathogens could provide significant public health benefits.
Finally, public education on the correct use of alcohol-based disinfectants can maximize their benefits and prevent misuse, which could contribute to the development of resistant bacterial strains. Understanding the correct concentrations and application methods is essential for effective microbial control.
Recognizing the impact of alcohol concentration on bacterial survival highlights the importance of precise formulation and application in disinfection practices. This knowledge not only informs healthcare protocols but also improves everyday practices in homes and communities around the world.
In conclusion, alcohol remains one of the most effective and versatile antimicrobial agents available. Its ability to disrupt bacterial membranes, denature proteins, and inhibit metabolic processes makes it a powerful tool in infection control and hygiene. Optimal alcohol concentrations ensure maximum bacterial killing while minimizing potential drawbacks such as resistance or toxicity. By continuing to study and apply these principles, we can enhance public health measures and further reduce the burden of bacterial infections.

Did You Enjoyed? So please Leave a comment for US 🙂