ITEACH.TOP | LEARN EVERYTHING
Introduction to Organ Transplantation: Concepts and Ethics
Organ transplantation is a lifesaving medical procedure that involves transferring organs or tissues from one body to another. While the concept of organ replacement has ancient origins, modern techniques have significantly advanced over the last century, offering hope to many patients with terminal organ failure. Organ transplantation is grounded in rigorous clinical standards and ethical principles, ensuring that both donor and recipient are treated with care and respect. Essential to understanding this domain is the discussion of medical necessity, donor compatibility, and the mechanisms involved in transplant validation.
From a moral perspective, organ transplantation raises important questions regarding the allocation of scarce medical resources, the rights of donors, and the obligations of society. Organ donation can be conducted from living or deceased donors, each with distinct ethical considerations. Living donors can donate a kidney or part of a liver, while deceased donors can provide multiple organs, potentially saving numerous lives. The ethical principles guiding organ transplantation include beneficence, non-maleficence, autonomy, and justice. These principles help ensure that the process respects human dignity and maximizes social benefit.
Kidney Transplantation: Process and Success Rates
Kidney transplantation remains one of the most common and successful types of organ transplantation procedures. The kidney is a vital organ responsible for filtering waste from the bloodstream and producing urine. Patients with end-stage renal disease (ESRD) often require a transplant to improve their survival and quality of life. The transplant process involves detailed evaluations of both the recipient and donor to ensure compatibility and reduce the risk of rejection.
Live kidney donation has become more accepted, accounting for a significant proportion of transplants. A healthy donor can lead a normal life with a single kidney, while the recipient often sees marked improvements in health and longevity. Advances in surgical techniques, immunosuppressive therapies, and post-operative care have greatly enhanced success rates, with many recipients experiencing more than a decade of function from their new organ. Despite these advancements, challenges such as organ shortage and long waiting lists persist.
Liver Transplantation: Advances and Challenges
Liver transplantation offers a curative option for patients with chronic liver disease, acute liver failure, and certain hepatic malignancies. The liver’s unique regenerative ability allows segmental liver transplants, where a portion of the liver is transplanted, benefiting both adult and pediatric recipients. Advances in surgical precision, perioperative care, and immunosuppressive treatments have decreased mortality rates and improved long-term outcomes.
However, liver transplantation poses significant challenges, including the complex management of cirrhosis, post-operative infections, and organ rejection. Allocation systems prioritize the sickest patients first, which can complicate the timing and success of the surgery. Efforts to expand the donor pool include split liver transplants, living donor liver transplants, and utilizing previously discarded marginal organs through better preservation techniques. Nevertheless, the demand for livers far exceeds supply, underscoring the need for innovative solutions and enhanced public awareness to increase donor registrations.
Heart Transplantation: Procedures and Long-Term Outcomes
Heart transplantation is a critical intervention for patients with end-stage heart failure or severe coronary artery disease unresponsive to other treatments. The procedure replaces a diseased heart with a healthy one from a deceased donor. Before transplantation, candidates undergo extensive evaluations to confirm the suitability of the transplant and to prepare for post-operative care.
Long-term outcomes for heart transplant recipients have improved through better surgical techniques, innovative immunosuppressive drugs, and comprehensive follow-up care. Survival rates have steadily increased, with many patients living 10 years or more post-transplant. Challenges include managing chronic rejection, infections due to immunosuppression, and complications from the surgery itself. Ongoing research focuses on xenotransplantation, mechanical circulatory support, and regenerative medicine to bridge the gap between the need for donor hearts and their availability.
Lung Transplantation: Indications and Complications
Lung transplantation becomes necessary for patients with devastating pulmonary conditions such as cystic fibrosis, chronic obstructive pulmonary disease (COPD), or idiopathic pulmonary fibrosis. This procedure can involve replacing one or both lungs, depending on the severity and nature of the disease. Determining candidacy involves a meticulous assessment of disease progression, physical condition, and ability to withstand the rigorous post-operative regimen.
Pulmonary function improvement post-transplant can significantly enhance the patient’s quality of life. Nevertheless, lung transplantation brings unique challenges, including a high susceptibility to infections, rejection, and chronic lung allograft dysfunction (CLAD). Compared to other organ transplants, lung recipients have a lower long-term survival rate, which underlines the need for ongoing advancements in surgical techniques, patient management, and immunosuppressive treatments.
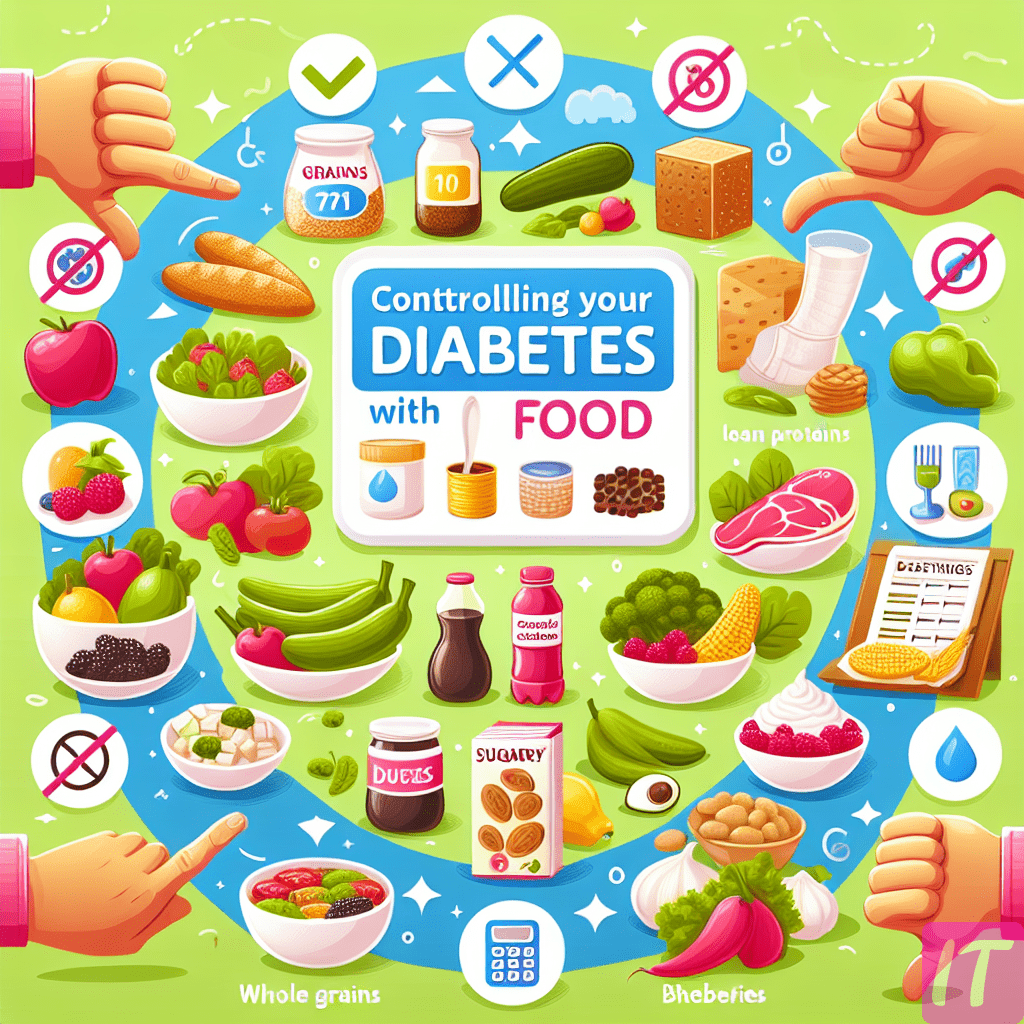
Pancreas Transplantation: Treatment for Diabetes
Pancreas transplantation can be a viable treatment option for patients with type 1 diabetes mellitus experiencing significant complications such as hypoglycemic unawareness or severe insulin resistance. The transplantation of a healthy pancreas or pancreas-islet cells can restore insulin production and glucose regulation, potentially offering a cure for diabetes.
This complex procedure often accompanies a kidney transplant in diabetic patients with renal failure. The dual transplantation addresses both the endocrine and renal complications of diabetes, improving overall patient outcomes. Despite its promise, pancreas transplantation involves significant risks, including rejection, pancreatitis, and complications from immunosuppressive drugs. Progress in organ preservation, surgical techniques, and post-transplant care continue to enhance patient prognosis and widen the eligibility criteria for transplantation.
Intestinal Transplantation: Addressing Short Bowel Syndrome
Intestinal transplantation is a life-saving option for patients with severe intestinal failure and complications from total parenteral nutrition (TPN), such as liver disease. This transplant aims to restore normal digestive functions in patients with short bowel syndrome or other irreversible intestinal conditions.
Success in intestinal transplantation heavily depends on meticulous surgical procedures, effective immunosuppression, and vigilant post-operative care. Despite its potential to significantly improve the quality of life, this procedure is fraught with challenges such as rejection, infections, and the high complexity of the pre- and post-operative management. Innovations in donor organ preservation, immunosuppressive regimens, and surgical techniques hold promise for improving outcomes and expanding the indications for this intricate procedure.

Corneal Transplantation: Restoring Vision
Corneal transplantation, or keratoplasty, is performed to restore vision in patients with corneal diseases, injuries, or degenerative conditions like keratoconus. This procedure involves replacing the damaged corneal tissue with a healthy donor cornea, allowing the restoration of clear vision.
Corneal transplantation has a high success rate due to the cornea’s immune privilege, reducing the risk of rejection. Several types of corneal transplants, including penetrating keratoplasty, endothelial keratoplasty, and deep anterior lamellar keratoplasty, are tailored to address specific corneal issues. Advances in microsurgical techniques, donor tissue preservation, and post-operative care have improved visual outcomes and graft survival rates, significantly enhancing patients’ lives.
Bone Marrow Transplantation: Treatment for Blood Disorders
Bone marrow transplantation (BMT), also known as hematopoietic stem cell transplantation, is a critical treatment for patients with blood disorders such as leukemia, lymphoma, and aplastic anemia. This procedure involves replacing diseased bone marrow with healthy stem cells, which can regenerate and restore normal blood cell production.
There are two primary types of BMT: autologous, where the patient’s own stem cells are used, and allogeneic, where a donor’s stem cells are transplanted. The success of BMT hinges on finding a compatible donor, typically a sibling or an unrelated donor matched through global registries. Despite its potential to cure severe blood disorders, BMT carries significant risks, including graft-versus-host disease (GVHD), infections, and transplant-related mortality. Continuing research aims to improve donor matching, reduce complications, and enhance long-term outcomes for patients undergoing this life-changing procedure.
Skin Transplantation: Healing Severe Burns and Injuries
Skin transplantation, or skin grafting, is a vital procedure for treating severe burns, traumatic injuries, and chronic non-healing wounds. This process involves transplanting healthy skin from a donor site to a damaged area, promoting healing and reducing the risk of infection.
There are two main types of skin grafts: split-thickness, involving the epidermis and part of the dermis, and full-thickness, including both layers. The choice depends on the extent and location of the injury. Skin grafting can provide both functional and aesthetic benefits, improving the patient’s quality of life. Challenges include graft rejection, infection, and the complexity of managing extensive burn injuries. Innovations in skin substitutes, tissue engineering, and improved surgical techniques are continually advancing the field, offering better outcomes for patients in need.
Understanding the Feasibility of Brain Transplantation
The hypothetical concept of brain transplantation involves transferring a person’s brain into another body. While this idea captivates the imagination, it faces monumental scientific and ethical challenges. The brain is the most intricate and least understood organ, responsible for consciousness, memory, and identity. Connecting a transplanted brain to the host body’s spinal cord, vasculature, and immune system poses unprecedented medical hurdles.
Currently, the field of neuroscience has not reached a level where such an endeavor is feasible. Significant obstacles include the reattachment of severed spinal cords, the rejection of foreign neural tissue, and the maintenance of brain function during transplantation. While advancements in neural biology and regenerative medicine continue to push boundaries, brain transplantation remains within the realm of theoretical exploration rather than practical application.
Ethical Considerations in Human Brain Transplantation
Brain transplantation raises profound ethical issues that extend beyond the typical concerns associated with organ transplantation. The brain is intimately tied to an individual’s identity, personality, and consciousness. Transplanting a brain into another body challenges the core concepts of self, posing questions about the continuity of personal identity and the moral status of such an entity.
Ethical considerations also involve the rights and welfare of both the donor and the recipient. The procedure’s experimental nature raises concerns about consent, the risk of exploitation, and the potential psychological impact on the individual undergoing the transplant. Additionally, the social implications of brain transplantation, such as potential disparities in access and the definition of death, require careful deliberation. As such, any future attempts must be guided by rigorous ethical frameworks and multidisciplinary dialogues.
Current Research and Developments in Brain Transplantation
Research in the realm of brain transplantation is primarily theoretical, focusing on understanding brain physiology, neural connectivity, and regenerative techniques. Key areas of investigation include spinal cord injury repair, neural plasticity, and the development of neuroprosthetics that can interface effectively with the brain.
Advancements in stem cell therapy, tissue engineering, and biocompatible materials are paving the way for potential breakthroughs. While these technologies aim to repair and regenerate brain tissues or restore functions lost due to injury, the leap to full brain transplantation remains far off. The research is progressively illuminating the complexities of the brain and central nervous system, providing valuable insights that may one day inform the feasibility of more radical interventions.
Neurological Implications of Brain Transplantation
The neurological implications of brain transplantation are profound, involving the reestablishment of functional neural networks and integration with the host body. Critical hurdles include reconnecting the brain to the spinal cord, re-establishing neural pathways, and ensuring appropriate blood supply and immune protection.
Current neuroscience suggests that even slight disruptions to neural connectivity can have devastating effects on cognitive and motor functions. Moreover, the brain’s vulnerability during transplantation—due to potential ischemia or immune responses—underscores the need for exceptionally advanced medical technologies. Understanding these implications is essential for any future attempts to bridge the gap between brain transplantation theory and clinical reality.
Immunological Challenges in Organ Transplantation
Organ transplantation invariably triggers immune responses, as the body recognizes the transplanted organ as foreign and mounts an attack against it. This immune response can lead to graft rejection, a primary concern in transplant medicine. Understanding and mitigating this response is crucial for transplant success.
Advances in immunosuppressive therapies have significantly improved the outcomes of organ transplants. These medications help to suppress the recipient’s immune system, reducing the likelihood of rejection. However, long-term use of immunosuppressants comes with risks such as increased susceptibility to infections and certain cancers. Research continues to seek a balance between effective immunosuppression and minimizing such adverse effects, aiming for tolerance where the body accepts the graft without ongoing medication.

The Role of Anti-Rejection Medications in Transplant Success
Anti-rejection medications, or immunosuppressants, are pivotal in the success of organ transplantation. These drugs work by dampening the recipient’s immune response to the foreign organ, preventing acute and chronic rejection. Commonly used medications include calcineurin inhibitors (like cyclosporine and tacrolimus), antiproliferative agents (like mycophenolate mofetil), and corticosteroids.
The development and refinement of these medications have transformed transplant medicine, allowing for higher success rates and longer graft survival. Careful management of immunosuppressive regimens is essential to balance the efficacy with the side effects, such as nephrotoxicity, hypertension, and susceptibility to infections. Ongoing research aims to develop more targeted therapies with fewer side effects and explore strategies for inducing immune tolerance to transplant recipients.
Psychological Impact of Organ Transplantation on Recipients
The psychological impact of organ transplantation on recipients is profound and multifaceted. Patients often experience a range of emotions, from relief and gratitude for receiving a life-saving organ to anxiety and guilt over the donor’s death. Long-term psychological support is crucial to address issues such as post-traumatic stress, depression, and anxiety.
The emotional well-being of transplant recipients plays a critical role in their recovery and overall quality of life. Pre- and post-transplant counseling, peer support groups, and mental health interventions are essential components of comprehensive transplant care. Understanding and addressing the psychological dimensions of organ transplantation can enhance patient outcomes, aiding in both physical and emotional recovery.
Improving Organ Donation Rates: Strategies and Policies
Improving organ donation rates is essential to address the persistent shortage of available organs for transplantation. Strategies to increase donor registrations include public education campaigns, incentivizing donations, and implementing opt-out policies, where individuals are presumed donors unless they explicitly opt out.
Effective policies prioritize transparency, equity, and respect for donor and recipient rights. Educating healthcare professionals about the importance of organ donation and effective communication with potential donor families can also boost donation rates. Collaborative efforts between governments, non-profits, and medical institutions are crucial to creating a supportive infrastructure that facilitates organ donation and addresses barriers such as cultural beliefs, misinformation, and logistical challenges.
Future Directions in Organ Transplantation Research
The future of organ transplantation research holds great promise with ongoing innovations in regenerative medicine, gene editing, and bioengineering. Techniques such as 3D bioprinting and organoid culture aim to create bioartificial organs, potentially eliminating the need for donor organs. Advances in xenotransplantation, using animal organs for human transplants, are also being explored to address organ shortages.
Gene editing technologies like CRISPR may offer solutions to immune rejection by modifying donor organs to be more compatible with human recipients. Additionally, research into immune tolerance aims to enable recipients to accept transplanted organs without lifelong immunosuppression. These groundbreaking developments, while still in experimental stages, signify a transformative shift towards more sustainable and effective transplant therapies.
Case Studies of Organ Transplant Successes and Failures
Case studies provide invaluable insights into the complexities and outcomes of organ transplantation. Success stories highlight the advancements in medical technology and patient care, demonstrating significant improvements in patient quality of life and survival rates. For example, kidney and liver transplants often result in long-term donor organ function and patient survival for over a decade.
Conversely, case studies of transplant failures shed light on the challenges and limitations of current practices. Instances of graft rejection, complications from immunosuppressive drugs, and post-operative infections underscore the need for ongoing research and innovation. These case studies are essential for understanding the multifaceted nature of organ transplantation, guiding future improvements in surgical techniques, patient management, and therapeutic interventions.
Conclusion
Organ transplantation represents a miraculous convergence of medical science, ethics, and human compassion. As we harness ever-evolving technologies and deepen our understanding of biological systems, the potential to save and enhance lives through transplantation continues to grow. From the transplantation of kidneys and hearts to